If the hospital lab is down, could you tell the difference between strep throat and mononucleosis by examing a patient’s blood? Could you differentiate between viral and bacterial pneumonia? Would you be able to determine if a patient is anemic and the likely cause?
Once upon a time doctors did complete blood counts in their own labs. In the future, we may do so again. Today’s article is contributed by Pete Farmer, who holds advanced degrees in research biology and history, and is also an RN and EMT. For Part I of the series, click HERE.
* * *
Introduction
Today, if you have blood drawn or some other specimen taken at the office of your primary care physician (PCP), chances are that it is sent out for diagnostic testing and analysis at LabCorp, Qwest Diagnostics, or one of their peers in the diagnostic testing industry. These companies have much to offer in terms of economies of scale, expertise, per unit cost savings, and specialized clinical and technical knowledge. In many ways, they have simplified the lives of doctors and patients alike. However, such firms have not always handled diagnostics for the typical family physician; in the not-so-recent past, many clinics did laboratory analysis and simple diagnostic work on-site. Most physicians – and many nurses – knew how to do a gram stain, a complete blood count, a determination of occult (fecal) blood, and other comparatively simple tests. These were done in a clinical lab right in the physician’s office or clinic. Since the passage of the Clinical Laboratory Improvement Amendments in 1988, however, such on-site testing has become rare – since CLIA certification is required before a given PCP can do in-house clinical lab tests covered under the act.
CLIA regulations have undoubtedly tightened laboratory standards, standardized procedures, and elevated the level of patient safety; these are worthwhile ends. However, these benefits have not come without costs. Because most PCPs now send out lab work they formerly did themselves – or had done by their staffs – front-line healthcare personnel have seen their laboratory skills atrophy from lack of use.
Anyone wishing to have back-up skills in case a high-tech clinical laboratory isn’t available, or simply wishing to be medically-prepared, might benefit from a review of some of the basic clinical lab tests that used to be commonly-done in physician offices. In the last installment (Part IV), we covered the basic Gram Stain and its use in typing different bacteria during light microscopy. In this installment, we will address another clinically-useful test employing the light microscope, namely the CBC (complete blood count). Before the advent of automated analyzers, when a physician ordered a CBC, and a patient’s blood was drawn, it was ultimately counted by a hematology medical lab technician, using a light microscope, a device called a Hemocytometer, and some simple supplies and reagents. Although using a hemocytometer to do a CBC isn’t considered state of the art any longer (in most cases, anyway), this method still works well if employed correctly and carefully.
In order to understand the utility of the hemocytometer, it is necessary to know some basic hematology (hematology is the study of blood, the blood forming organs, and diseases of the blood – as well as diagnosis and treatment of such disorders). Specifically, what is a complete blood count, and why is it clinically useful for the diagnostician? Under what clinical circumstances would a CBC be indicted for a patient? It gets more complicated still, because in order to do a CBC, one must be able to collect a blood sample without contaminating or degrading it; additional chemical treatment may be required if the sample is to be stored or transported. Whole blood must be pretreated chemically before a CBC is done. This gets us into the realm of clinical chemistry – which means having the appropriate laboratory glassware, reagents, and other supplies. Finally, being able to draw, preserve and process blood, and do a CBC with a hemocytometer correctly – is of little use if you do not know what the results mean.
Before getting a migraine headache about all of this, and getting intimidated, take a deep breath and remember that a stepwise approach to acquiring new knowledge is the way to proceed. In the following article and installments to come, we’ll examine each of the following sub-sections and how they fit into performing a valid and clinically-useful CBC.
Venipuncture
Clinical Chemistry of Blood
The Complete Blood Count
The Hemocytometer
Interpreting the results of a CBC
Blood: Anatomy, Physiology and Clinical Chemistry – Some basics

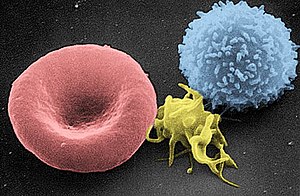
Image via Wikipedia
Hematology is a mature and varied field of medical science; scientists and physicians can and do spend entire careers specialized in diseases of the blood. For our purposes, we will keep things as simple as possible – but still endeavor to hit the high points. Please note that the following discussion does not replace college-level study in anatomy and physiology, chemistry, biology, physics or related fields. If one desires an in-depth understanding of blood, extensive study in these areas will be necessary.
What is blood and what are its functions? Blood is a specialized fluid that delivers necessary oxygen and nutrients to the body’s cells and tissues, and removes metabolic and other waste products, such as carbon dioxide, from the same cells.
Blood is composed of specialized cells of several types, suspended in plasma, which is the liquid fraction of blood. Plasma comprises ~ 55% of total blood volume, and is itself 93% water. Plasma also contains proteins, glucose, clotting factors, ionic minerals, hormones and carbon dioxide. In humans, blood cells (or hematocytes) fall within three broad categories – red blood cells (erythrocytes), white blood cells (leukocytes) and platelets (thrombocytes). White blood cells (WBCs) are further divided into subtypes dependent on appearance, function, and other factors; these include neutrophils, eosinophils, basophils, lymphocytes and monocytes – as well as macrophages and dendritic cells. WBCs can be characterized as granular or agranular.
An adult weighing 160 lbs. will have roughly 4.7 liters (5 quarts) of blood volume, or 1/11th of a given body weight. An eighty pound child has half that amount, while an 8-lb. infant has 8.5 fluid ounces of blood. Adults living at high altitude may have as much as 1.9 L more blood than those living at/near sea level. Blood is pumped through the circulatory system, which is comprised of the heart, blood vessels (arteries, veins, capillaries), and lymphatic system.
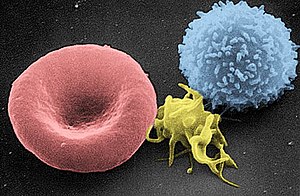
Image via Wikipedia
Blood can be thought of as a complex chemical solution in which various solids and gases are dissolved, and move simultaneously with the other constituents of blood. As such, the chemical and physical properties of blood are homeostically regulated to fall within specific ranges in the healthy individual. In the disease state, these values are displaced in characteristic ways – allowing the clinician and pathologist to use blood tests to make diagnoses. Blood pH is optimally 7.35 – 7.45 or slightly alkaline. The concentration of dissolved blood gases falls within specific physiological ranges for partial pressures for oxygen, carbon dioxide, as well as bicarbonate and other gases. Oxygen is transported primarily via hemoglobin in red blood cells, while CO2 is transported in solution in the plasma.
[Image shows, left to right, a red blood cell, a platelet, and a small white blood cell, under scanning electron microscopy. – Doc Cindy]
Coming next: blood collection
Copyright © 2011 Peter Farmer