-
Active ingredient: Azithromycin
- Common brand names: Zithromax, Sumamed, Azasite
- Drug class: Antibiotic, Macrolide, Azalide group
- Pregnancy Category: B
- Habit forming? No
- Originally discovered: 1981, Pliva, Croatia
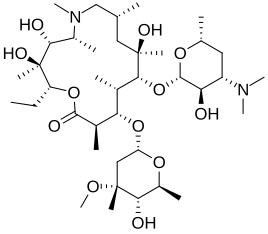
Azithromycin is the first macrolide antibiotic belonging to the azalide group. Azithromycin is derived from erythromycin by adding a nitrogen atom into the lactone ring of erythromycin A. Azithromycin is sold under the brand names Zithromax and Sumamed, and is one of the world’s best-selling antibiotics.
Since the 1970s, PLIVA’s (Croatian pharmaceutical company, based in Zagreb, Croatia) research team, led by Dr Slobodan Dokic, had been working in the area of macrolide antibiotics1. In 1981, his team of researchers, Gabrijela Kobrehel, Zrinka Tamburasev and Gorjana Radobolja-Lazarevski, synthesised a novel antibiotic named azithromycin, the first member of a new class of macrolide antibiotics, termed azalides. Azithromycin dihydrate was obtained from the erythromycin molecule and demonstrated superior properties.
It was patented in 1981, and was later found by Pfizer’s scientists while going through patent documents. In 1986 Pliva and Pfizer signed a licensing agreement which gave Pfizer exclusive rights for the sale of azithromycin in Western Europe and the United States. Pliva brought their azithromycin on the market in Central and Eastern Europe under the brand name of Sumamed in 1988, and Pfizer under the brand name Zithromax in 1991.
Because of its exceptional therapeutic properties, azithromycin revolutionised antibiotic treatment and became one of the most successful drugs worldwide. From its early trials, it proved to be an extremely efficient antibiotic with expanded and enhanced antibacterial activity (particularly against gram-negative pathogens), prolonged and higher tissue concentration and a low incidence of gastrointestinal side effects compared to other similar antibiotics.
Azithromycin is indicated for the treatment of the following infections due to susceptible strains of sensitive organisms:
- Upper respiratory tract infections: pharyngitis/tonsillitis, sinusitis, otitis media
- Lower respiratory tract infections: bronchitis, acute exacerbation of chronic bronchitis, community acquired pneumonia of mild severity.
- Sexually transmitted diseases: uncomplicated urethritis, uncomplicated cervicitis due to Neisseria gonorrhoeae or Chlamydia trachomatis.
- Chancroid (genital ulcer disease in men).
- Skin and soft tissue infections: erysipelas, impetigo, secondary pyoderma, erythema migrans.
- Mycobacterial Infections.
Off-label and investigational uses of Azithromycin include:
Infectious diseases:
- Pelvic inflammatory disease (PID)
PID comprises a spectrum of inflammatory disorders of the upper female genital tract, including any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. Sexually transmitted organisms, Neisseria gonorrhoeae and Chlamydia trachomatis are the major pathogens causing PID. Azithromycin provides a short simple treatment option for PID3. - Infectious diarrhoea
Infectious diarrhoea is the most common cause of diarrhoea worldwide. Azithromycin is a good choice for pregnant women and children, for whom fluoroquinolones are not approved, and for patients who cannot otherwise tolerate fluoroquinolones4. - Dental infections
Azithromycin is given to people allergic to penicillins and those who have abscesses and other dental infections, especially those extending into the sinuses, gums and bone, and for whom other antibiotics have proved ineffective. - Acne
Acne vulgaris is a common inflammatory disorder of the skin. Azithromycin is a safe and effective alternative in the treatment of inflammatory acne with few side-effects.
A randomized study6 compared the efficacy of azithromycin with doxycycline. Facial lesions significantly improved with both drugs. Neither drug was shown to be more effective than the other. The beneficial effect continued until 2 months after treatment. This study indicates that azithromycin is at least as effective as doxycycline in the treatment of acne. - Pertussis
Azithromycin is as effective as and better tolerated than erythromycin for the treatment of pertussis7. - Prostatitis
Azithromycin is used in the treatment of chronic prostatitis caused by Chlamydia trachomatis and Neisseria gonorrhoeae. - Syphilis
Azithromycin has been successfully used as a multidose treatment in persons who have early syphilis8. - Mediterranean spotted fever (Rickettsiosis)
Mediterranean spotted fever, also known as boutonneuse fever, is transmitted by the dog tick Rhipicephalus sanguineus and has a characteristic rash and a distinct mark, a tache noire (black spot) at the site of the tick bite. Azithromycin is effective treatment in children and can be used as alternatives to doxycycline in adults9. - Endocarditis
Azithromycin is used for prophylaxis of bacterial endocarditis in persons who are allergic to penicillin and undergoing surgical or dental procedures10.
Non-infectious diseases:
- Atherosclerosis
Azithromycin appears to reduce the risk of Chlamydia pneumoniae-induced atherosclerosis11. - Cystic fibrosis
According to the studies2, azithromycin significantly improves quality of life, reduces the number of respiratory exacerbations, and reduces the rate of decline in lung function in persons with cystic fibrosis.
While the exact mechanisms are unknown, anti-inflammatory rather than antimicrobial properties of macrolides seem to be responsible for the beneficial effects.
Advantages:
- Excellent efficacy. Many scientific studies have shown that azithromycin is better or equally effective compared to other antibiotics.
- Low potential for drug interactions. Azithromycin, unlike the majority of macrolides, does not bind to cytochrome P-450 in the liver, resulting in low potential for drug to drug interaction.
- Low rate of side effects. Side effects with azithromycin are mild to moderate, mostly gastrointestinal.
- Sustained antimicrobial activity. Azithromycin reaches high and sustained tissue concentrations that results in sustained antimicrobial activity.
- Active against intracellular bacteria (Chlamydia pneumoniae, Chlamydia trachomatis, Mycoplasma pneumoniae, Legionella spp.). Since azithromycin is a weak base, it easily penetrates the cell membrane and stays within the cell.
- Targeted activity at the site of infection. Because of the transport with white blood cells, azithromycin possesses a unique property – targeted activity at the site of infection. In infected tissues, azithromycin achieves high and sustained therapeutic concentrations that last five to seven days after the last dose.
- Suitable choice for empirical therapy. Since azithromycin has a good activity against the most common pathogens it is used as a choice for empirical therapy.
- Good compliance: short once daily dosing regimen. Azithromycin’s short dosing regimen is convenient and improves patient compliance. For the majority of infections, azithromycin is administered once daily for three days. In the treatment of sexually transmitted diseases, azithromycin is administered as a single dose.
- Active against most respiratory tract infections. Betalactams lack activity against atypical pathogens. Among macrolides, azithromycin shows the best activity against H. influenzae.
Disadvantages:
- Food reduces azithromycin absorption rate. Azithromycin capsules should not be mixed with or taken with food, however tablets may be taken without regard to food.
Azithromycin acts by interfering with bacterial protein synthesis. Although this mechanism is considered bacteriostatic, concentrations several times higher than minimum inhibitory concentrations (MIC) contribute to the bactericidal activity of azithromycin.
Non-antibiotic properties: immunomodulating effect
Data indicate that macrolides may have immunomodulatory activities: in vitro and ex vivo studies clearly show that macrolides can influence cytokine production by several cell types; furthermore, macrolides can alter polymorphonuclear cell functions in vitro and ex vivo. Although immunomodulation may serve as one explanation for the beneficial effects of macrolides in patients with chronic pulmonary inflammation, the effect of low-dose macrolide therapy on biofilm-formation may form a second explanation for the positive effects of long-term low-dose macrolide therapy.
The half-life of Azithromycin is about 68 hours. So it takes about 16-17 days to clear out of the system.
Chlamydia trachomatis is the most common sexually transmitted infection worldwide, especially among adolescents and young adults. Chlamydia is a very guileful infection because many cases of infection are asymptomatic. Untreated infection can progress to persistent infection, which may initiate pelvic inflammatory disease, ectopic pregnancy, tubal factor infertility, and chlamydia-induced arthritis.
The importance of azithromycin comes from its highly favorable pharmacokinetic properties: acid stability, high tissue penetration, low serum levels and a very long half-life. Anti-chlamydial levels of the drug are readily achieved inside cells or tissues. Adequate intracellular levels may be sustained for several days because of the slow efflux from cells.
According to the CDC Guidelines azithromycin is a first-line treatment for chlamydial genital infections. Azithromycin is also recommended by the CDC for the treatment of pregnant women.
The treatment consists of a single 1 gram dose.
Recurrent Chlamydia
Relapsing or persistent chlamydia is a common problem, even though patients are often treated appropriately. Azithromycin may be particularly effective against persistent infection4.
- 1. SUMAMED – success story, from sumamed.com.hr
- 2. Wolter J, Seeney S, Bell S, Bowler S, Masel P, McCormack J. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax. 2002 Mar;57(3):212-6.
- 3. Bevan CD, Ridgway GL, Rothermel CD. Efficacy and safety of azithromycin compared with two standard multidrug regimens for the treatment of acute pelvic inflammatory disease. J Int Med Res. 2003 Jan-Feb;31(1):45-54. PubMed
- 4. Reveneau N, Crane DD, Fischer E, Caldwell HD. Bactericidal activity of first-choice antibiotics against gamma interferon-induced persistent infection of human epithelial cells by Chlamydia trachomatis. Antimicrob Agents Chemother. 2005 May;49(5):1787-93.
- 5. Khan WA, Seas C, Dhar U, Salam MA, Bennish ML. Treatment of shigellosis. Ann Intern Med. 1997 May 1;126(9):697-703. PubMed
- 6. Kus S, Yucelten D, Aytug A. Comparison of efficacy of azithromycin vs. doxycycline in the treatment of acne vulgaris. Clin Exp Dermatol. 2005 May;30(3):215-20. PubMed
- 7. Langley JM, Halperin SA, Boucher FD, Smith B; Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC). Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics. 2004 Jul;114(1):e96-101.
- 8. Riedner G, Rusizoka M, Todd J, Maboko L, Hoelscher M, Mmbando D, Samky E, Lyamuya E, Mabey D, Grosskurth H, Hayes R. Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N Engl J Med. 2005 Sep 22;353(12):1236-44.
- 9. Dzelalija B, Petrovec M, Avsic-Zupanc T, Strugar J, Milic’ TA. Randomized trial of Zithromax in the prophylaxis of Mediterranean spotted fever. Acta Med Croatica. 2002;56(2):45-7. PubMed
- 10. Rouse MS, Steckelberg JM, Brandt CM, Patel R, Miro JM, Wilson WR. Efficacy of azithromycin or clarithromycin for prophylaxis of viridans group streptococcus experimental endocarditis. Antimicrob Agents Chemother. 1997 Aug;41(8):1673-6.
- 11. Bouwman JJ, Visseren FL, Bevers LM, van der Vlist WE, Bouter KP, Diepersloot RJ. Azithromycin reduces Chlamydia pneumoniae-induced attenuation of eNOS and cGMP production by endothelial cells. Eur J Clin Invest. 2005 Sep;35(9):573-82. PubMed
Published: March 31, 2008
Last updated: October 25, 2010
Azithromycin (Zithromax) versus Other Medications
- Pneumonia
Azithromycin (3-day, once-daily course) is as effective and well tolerated as clarithromycin (10-day, twice-daily course) in the treatment of mild to moderate community-acquired pneumonia.
Randomized, multicentre study7 compared azithromycin versus clarithromycin in the treatment of adults with mild to moderate community-acquired pneumonia. A satisfactory clinical response was recorded at the end of therapy in 83 of 88 (94%) evaluable azithromycin-treated and 84 of 88 (95%) evaluable clarithromycin-treated patients. At day 19-23, only one patient in each treatment group had relapsed. Thirty-one of 32 (97%) pathogens isolated from patients in the azithromycin group were eradicated, compared with 32 of 35 (91%) isolated from clarithromycin patients. Incidences of treatment-related adverse events were similar for the two groups. Two (2%) clarithromycin patients discontinued therapy due to severe treatment-related adverse events; none in the azithromycin group did. - Acute exacerbation of chronic bronchitis
Three-day treatment with azithromycin 500 mg once daily is equivalent to a 10-day treatment with clarithromycin 500 mg twice daily in adults with acute exacerbation of chronic bronchitis (AECB).
Randomized, double-blind, multicenter study6 compared the efficacy and safety of oral azithromycin 500 mg once daily for 3 days with those of oral clarithromycin 500 mg twice daily for 10 days. The clinical cure (based on direct observation of the patient) rates were equivalent in the two treatment groups at 85% with azithromycin and 82% with clarithromycin. Bacteriologic success rates were also equivalent between the azithromycin and clarithromycin treatment groups at test of cure for S. pneumoniae (90.6% and 85.2%, respectively), H. influenzae (71.4% and 81.3%, respectively) and M. catarrhalis (100% and 86.7%, respectively). The overall incidence of treatment-related adverse events was similar in the azithromycin and clarithromycin groups (20.9% and 26.8%, respectively), with the most common being abdominal pain (6.3% and 6.1%, respectively), diarrhea (4.4% and 5.5%, respectively), and nausea (4.4% and 3.7%, respectively). - Otitis media (infection of the middle ear)
Both azithromycin and clarithromycin are effective for the treatment of children with acute otitis media.
A randomized, open clinical trial8 compared the efficacy, safety and tolerance of azithromycin and clarithromycin in pediatric patients with acute otitis media. Of 100 patients enrolled, 97 were considered evaluable. The most common middle ear pathogens were Streptococcus pneumoniae (60%), Haemophilus influenzae (15%) and Staphylococcus aureus (13%). Fifty patients (100%) treated with azithromycin and 45 (95.7%) patients treated with clarithromycin had a satisfactory clinical response. Rates of persistence of middle ear effusion and possible drug related side effects were comparable.
- Chlamydia trachomatis infections
In clinical trials2, the bacteriological cure rate of single dose azithromycin 1000 mg (95 to 100%) was similar to that of oral doxycycline 200 mg/day for 7 days (88 to 100%).
However, according to the recent research1 Azithromycin may be particularly effective against persistent chlamydial infection. In contrast, doxycycline may not be as effective in treating persistent infection.
Chronic chlamydial infections such as pelvic inflammatory disease or trachoma involve persistent infection and uncomplicated infections are a mixture of acute and persistent infections. Therefore azithromycin would be more effective for the treatment of chlamydial infections than doxycycline1. - Endocervicitis
Both azithromycin and doxycycline are effective in the treatment of non-gonococcal endocervicitis.
Prospective-randomised study3 compared azithromycin versus doxycycline in the treatment of non-gonococcal mucopurulent endocervicitis. The eradication rate of bacteria in the azithromycin group was 71.4%, and 77.3% in the doxycycline group. - Acne
Azithromycin 500 mg once a day for four days per month appears to be as effective as daily doxycycline 100 mg4. - Lyme disease (Erythema migrans)
Azithromycin is equally effective as doxycycline in the treatment of Lyme disease.
A randomized, multicenter, open clinical trial5 compared the effectiveness of azithromycin and doxycycline in the treatment of Lyme disease associated with erythema migrans. Clinical success (based on direct observation of the patient) was observed in 95.8% azithromycin- and 82.5% doxycycline-treated patients.
- Acne
Azithromycin is at least as effective as minocycline in the treatment of facial comedonic and papulopustular acne.
An open study10 compared the clinical efficacy and tolerability of azithromycin and minocycline. Azithromycin was administered as a single oral dose (500 mg/day) for 4 days in four cycles every 10 days and minocycline was administered 100 mg daily for 6 weeks. Improvement was assessed 6 weeks after initiation of treatment with a four-graded scale. A satisfactory clinical response was observed in 75.8% of the patients treated with azithromycin and in 70.5% of those treated with minocycline. Both agents were well tolerated and mild side effects were reported in 10.3% of azithromycin and 11.7% of minocycline treated patients.
- Chlamydia infection
Chlamydia infection during pregnancy. Both amoxicillin and azithromycin are effective in the treatment of cervical Chlamydia trachomatis infection during pregnancy. However, azithromycin seems to have a lower rate of recurrent infection12. Amoxicillin is slightly better tolerated than azithromycin.
In a randomized controlled trial11 comparing amoxicillin and azithromycin there was similar treatment efficacy between amoxicillin and azithromycin (58% vs 64%, respectively). In the study 5.5% of women were intolerant to amoxicillin, compared with 10.9% to azithromycin. - Otitis media
Single dose azithromycin is as effective as high dose amoxicillin for 10 days for the treatment of children with otitis media. Diarrhea occurs more frequently with amoxicillin therapy than with azithromycin.
In a randomized, multicenter, double blind trial13 children (6-30 months of age) with acute otitis media (AOM) were randomized to treatment with single dose azithromycin (30 mg/kg) or high dose amoxicillin (90 mg/kg/d, in 2 divided doses) for 10 days. The clinical success rates for azithromycin and amoxicillin were comparable for all patients (84% and 84%, respectively) and for children < or =2 years of age (82% and 82%, respectively). The clinical efficacies among all microbiologic modified intent-to-treat evaluable subjects were comparable for patients treated with azithromycin (80%) and patients treated with amoxicillin (83%). The rates of side effects for azithromycin and amoxicillin were 20% and 29%, respectively. Diarrhea was more common with amoxicillin therapy than with azithromycin (17.5% and 8.2%, respectively). Compliance was higher in the azithromycin group (100%) than in the amoxicillin group (90%). - Lyme disease
Amoxicillin is more effective than azithromycin for erythema migrans.
In a double-blind, randomized, controlled trial14 patients treated with amoxicillin were significantly more likely than those treated with azithromycin to achieve complete resolution of disease at day 20, the end of therapy (88% compared with 76%). More azithromycin-treated patients (16%) than amoxicillin-treated patients (4%) had relapse. For patients treated with azithromycin, development of an antibody response increased the possibility of achieving a complete response (81% of seropositive patients achieved a complete response compared with 60% of seronegative patients). Patients with multiple erythema migrans lesions were more likely than patients with single erythema migrans lesions to have a positive antibody titer at baseline. Fifty-seven percent of patients who had relapse were seronegative at the time of relapse.
- Otitis media
Azithromycin and amoxicillin/clavulanate have similar efficacy in the treatment of acute otitis media in children. However, azithromycin is significantly better tolerated than amoxicillin/clavulanate.
Randomized, double-blind study15 compared azithromycin and amoxicillin/ clavulanate for the treatment of acute otitis media in children. One hundred and eighty-eight children (mean age 3.5 years) were randomized to azithromycin and 185 to co-amoxiclav. At day 10, the clinical success rate was 153/185 (83%) in children treated with azithromycin and 159/181 (88%) in children treated with co-amoxiclav. At day 28, 134/182 (74%) of the children were cured on azithromycin compared with 124/180 (69%) on co-amoxiclav. Also at day 28, signs of acute otitis media, such as abnormal reflectometry (45% versus 59%), bulging of the eardrum (10% versus 16%) and loss of tympanic membrane landmarks (11% versus 22%) were seen less frequently in azithromycin- than co-amoxiclav-treated children, respectively. Treatment-related side effects were seen in 11% of azithromycin patients compared with 20% on co-amoxiclav. - Sinusitis
Azithromycin and amoxicillin/clavulanate have similar efficacy in the treatment of sinusitis. However, azithromycin is better tolerated than amoxicillin/clavulanate.
Randomized double-blind study16 compared 3- and 6-day regimens of azithromycin with a 10-day amoxicillin-clavulanate regimen for treatment of acute bacterial sinusitis. Clinical success (based on direct observation of the patient) rates were equivalent among patients at the end of therapy (azithromycin 3 days, 88.8%; azithromycin 6 days, 89.3%; amoxicillin/clavulanate, 84.9%) and at the end of the study (azithromycin 3 days, 71.7%; azithromycin 6 days, 73.4%; amoxicillin/clavulanate, 71.3%). Patients treated with amoxicillin/clavulanate reported a higher incidence of treatment-related side effects (51.1%) than azithromycin-3 (31.1%) or azithromycin-6 (37.6%). More amoxicillin/clavulanate patients discontinued the study (n = 28) than azithromycin-3 (n = 7) and azithromycin-6 (n = 11). Diarrhea was the most frequent treatment-related side effect. - Lower respiratory tract infections
Azithromycin and amoxicillin/clavulanate have similar efficacy in the treatment of lower respiratory tract infections, but azithromycin is better tolerated than amoxicillin/clavulanate. An additional advantage of the azithromycin is the easy administration and short duration of therapy.
Multicentre randomized double-blind, double-dummy study17 compared the efficacy, safety and tolerability of a 3 day course of azithromycin with a 10 day course of co-amoxiclav in the treatment of children with acute lower respiratory tract infection. Of 110 patients, 56 and 54 patients, respectively, were treated with azithromycin or co-amoxiclav. The percentage of patients cured or clinically improved at days 10-13 (primary endpoint) was 91% for azithromycin and 87% for co-amoxiclav. This difference of 4% was not statistically significant. Significantly more treatment-related side effects were found in the co-amoxiclav group. This was largely due to a higher percentage (43% versus 19%) of gastrointestinal complaints.
- Streptococcal pharyngitis/tonsillitis
Azithromycin (10 or 20 mg/kg/day one daily for 3 days) is as safe and effective as penicillin V (4 times daily for 10 days) in the treatment of paediatric patients with acute pharyngitis/tonsillitis.
The efficacy and safety of azithromycin and penicillin V in the treatment of acute streptococcal pharyngitis/tonsillitis in paediatric patients were compared in a double-blind, double-dummy prospective study9. A satisfactory clinical response (cure or improvement) was recorded in 99% of the 10 mg/kg azithromycin group, 100% of the 20 mg/kg azithromycin group, and 97% of the penicillin V group at the end of therapy (day 12-14). At the follow-up evaluation (day 28-30), relapse rates in patients cured or improved at the end of therapy were 6%, 5%, and 2%, respectively. Bacteriological eradication rates at the end of therapy were 98% in both azithromycin groups and 92% in patients who received penicillin V; pathogen recurrence was recorded at follow-up in 4% of the 20 mg/kg azithromycin group and in 6% of both the 10 mg/kg azithromycin and penicillin V groups. Treatment-related adverse events, the majority of mild to moderate severity, occurred in 13% of patients in the 20 mg/kg azithromycin group, 9% in the 10 mg/kg azithromycin group, and 5% in the penicillin V group.
- Skin and skin structure infections
Azithromycin may be somewhat more effective than cefadroxil for treating uncomplicated skin and skin structure infections. Also, azithromycin is better tolerated.
Multicenter, investigator-blind study18 compared the efficacy and safety of azithromycin and cefadroxil for the treatment of uncomplicated skin and skin structure infections. Clinical and bacteriologic response was assessed between days 10 and 13 (primary end point) and between days 28 and 32. Clinical success (resolution of symptoms) rates assessed between days 10 and 13 were 97% (111/114) for azithromycin and 96% (101/105) for cefadroxil. For azithromycin and cefadroxil, corresponding rates of bacteriologic eradication for Staphylococcus aureus were 94% (64/68) and 86% (60/70), respectively, and for Streptococcus pyogenes, 80% (4/5) and 100% (6/6), respectively. Clinical success rates assessed between days 28 and 32 were 100% (82/82) for azithromycin compared with 90% (75/83) for cefadroxil. Corresponding rates of eradication for S aureus were 100% (59/59) versus 89% (56/63), respectively; and for S pyogenes, 100% (4/4) versus 83% (5/6), respectively. The incidence of treatment-related side effects was similar in the 2 treatment groups. However, 5 of the 139 patients (4%) in the cefadroxil group discontinued therapy because of treatment-related side effect compared with none of the 152 patients in the azithromycin group.
- Pneumococcal pulmonary infections.
Cefdinir or azithromycin have comparable effectiveness in the treatment of acute otitis media.
A multicenter, prospective, single-blind study19 compared cefdinir and azithromycin in children with acute otitis media. Three hundred fifty-seven patients were enrolled in the study. The majority of evaluable children (77%) had previously received conjugated heptavalent pneumococcal vaccine (PCV7) against Streptococcus pneumoniae. At the end-of-therapy visit, clinical cure (resolution of symptoms) rates were comparable for cefdinir and azithromycin (87%, [151/174] and 85% [149/176], respectively). In addition, clinical cure rates at the end-of-therapy visit in the children who had been vaccinated with PCV7 were comparable between cefdinir and azithromycin (86% vs 83%). No significant difference in clinical cure rates was observed at the follow-up visit (76% and 86%). Parental satisfaction was similar between treatment groups with regard to ease of use, taste, compliance, health care resource utilization, and missed days of work and day-care. Both antibiotics were well tolerated; diarrhea and abnormal stools were the most common antibiotic-related side effects.
- Exacerbations of chronic obstructive pulmonary disease
Both azithromycin and cefuroxime are effective treatments for exacerbations in patients with chronic obstructive pulmonary disease. Azithromycin has a lower rate of side effects.
A randomized study20 compared 3 days of azithromycin treatment and 10 days of cefuroxime treatment in exacerbations in patients with chronic obstructive pulmonary disease. 50 patients were treated with azithromycin and 51 with cefuroxime. The evolution of the symptoms was similar although with a trend to greater improvement in those treated with azithromycin. Functional and gasometric evolution was similar in the two schedules. Three patients treated with azithromycin required hospital admission, as did 5 treated with cefuroxime. A greater number of treatment-related side effects were observed in patients treated with cefuroxime (18%) than in those receiving azithromycin (10%), with gastrointestinal side effects being the most commonly observed.
- Chronic prostatitis (Chlamydia trachomatis)
Azithromycin is significantly more effective than ciprofloxacin 21.
Significantly higher eradication and a significantly higher clinical cure were achieved in the group of patients treated with azithromycin than in the ciprofloxacin group. - Shigellosis
Ciprofloxacin is somewhat more effective than azithromycin in the treatment of Shigellosis (a type of infective diarrhea) 22.
In a double-blind, randomized, controlled trial azithromycin therapy was clinically successful in 28 (82%) patients and ciprofloxacin therapy in 32 (89%) patients. Therapy was bacteriologically successful in 32 (94%) patients receiving azithromycin and 36 (100%) patients receiving ciprofloxacin. - Gonorrhea
1 g azithromycin is at least as effective and well tolerated as 500 mg of ciprofloxacin in the treatment of gonococcal infections. Azithromycin is particularly useful for sailors and people constantly on the move 23.
59 men and 49 women with gonococcal infection were enrolled in clinical study. Data of 50 patients treated with azithromycin and 51 with ciprofloxacin were evaluable for efficacy and tolerability at the end of the study. After 2 weeks clinical and microbiological cure rates were 96.0% (48 out of 50) for the patients treated with azithromycin and 92.15% (47 out of 51) for the patients treated with ciprofloxacin. Side effects were reported in 5 patients treated with azithromycin and 6 with ciprofloxacin.
- Acute bacterial exacerbations of chronic bronchitis
Standard 5-day course of oral azithromycin was clinically and bacteriologically equivalent to a 7-day course of oral levofloxacin in the treatment of ABECB. Favorable results were demonstrated in 89% of patients receiving azithromycin and in 92% of patients receiving levofloxacin by day 4 of therapy. At day 24 favorable responses were approximately 82% and 86%, respectively. The bacterial eradication rates of respiratory pathogens were 96% for azithromycin and 85% for levofloxacin24. Both treatments are well-tolerated, with the majority of adverse events being GI in nature. - Community-acquired pneumonia
A single 2 g dose of azithromycin microspheres is at least as effective as a 7-day course of levofloxacin in the treatment of mild to moderate community-acquired pneumonia25.
The cure rates were 89.7% for azithromycin microspheres and 93.7% for levofloxacin. Bacteriologic success at test of cure in the “bacteriologic per protocol” population was 90.7% for azithromycin microspheres and 92.3% for levofloxacin. Both medications were well tolerated. The incidence of side effects was 19.9% for azithromycin and 12.3% for levofloxacin. - Sinusitis
Single 2 g dose azithromycin microspheres has efficacy comparable to 10 days of levofloxacin in the treatment of acute bacterial sinusitis26.
Clinical success rates were 94.5% with azithromycin-microspheres and 92.8% with levofloxacin. In patients with Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis, clinical cure rates were 97.3%, 96.3%, and 100%, respectively, for the azithromycin and 92.3%, 100%, and 90.9%, respectively, for the levofloxacin.
- 1. Reveneau N, Crane DD, Fischer E, Caldwell HD. Bactericidal activity of first-choice antibiotics against gamma interferon-induced persistent infection of human epithelial cells by Chlamydia trachomatis. Antimicrob Agents Chemother. 2005 May;49(5):1787-93. PubMed
- 2. Lau CY, Qureshi AK. Azithromycin versus doxycycline for genital chlamydial infections: a meta-analysis of randomized clinical trials. Sex Transm Dis. 2002 Sep;29(9):497-502. PubMed
- 3. Sendag( F, Terek C, Tuncay G, Ozkinay E, Guven M. Single dose oral azithromycin versus seven day doxycycline in the treatment of non-gonococcal mucopurulent endocervicitis. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):44-7. PubMed
- 4. Parsad D, Pandhi R, Nagpal R, Negi KS. Azithromycin monthly pulse vs daily doxycycline in the treatment of acne vulgaris. J Dermatol. 2001 Jan;28(1):1-4. PubMed
- 5. Barsic B, Maretic T, Majerus L, Strugar J. Comparison of azithromycin and doxycycline in the treatment of erythema migrans. Infection. 2000 May-Jun;28(3):153-6. PubMed
- 6. Swanson RN, Lainez-Ventosilla A, De Salvo MC, Dunne MW, Amsden GW. Once-daily azithromycin for 3 days compared with clarithromycin for 10 days for acute exacerbation of chronic bronchitis: a multicenter, double-blind, randomized study. Treat Respir Med. 2005;4(1):31-9. PubMed
- 7. O’Doherty B, Muller O. Abstract Randomized, multicentre study of the efficacy and tolerance of azithromycin versus clarithromycin in the treatment of adults with mild to moderate community-acquired pneumonia. Azithromycin Study Group. Eur J Clin Microbiol Infect Dis. 1998 Dec;17(12):828-33. PubMed
- 8. Arguedas A, Loaiza C, Rodriguez F, Herrera ML, Mohs E. Comparative trial of 3 days of azithromycin versus 10 days of clarithromycin in the treatment of children with acute otitis media with effusion. J Chemother. 1997 Feb;9(1):44-50. PubMed
- 9. O’Doherty B. Azithromycin versus penicillin V in the treatment of paediatric patients with acute streptococcal pharyngitis/tonsillitis. Paediatric Azithromycin Study Group. Eur J Clin Microbiol Infect Dis. 1996 Sep;15(9):718-24. PubMed
- 10. Gruber F, Grubisic’-Greblo H, Kastelan M, Brajac I, Lenkovic’ M, Zamolo G. Azithromycin compared with minocycline in the treatment of acne comedonica and papulo-pustulosa. J Chemother. 1998 Dec;10(6):469-73. PubMed
- 11. Jacobson GF, Autry AM, Kirby RS, Liverman EM, Motley RU. A randomized controlled trial comparing amoxicillin and azithromycin for the treatment of Chlamydia trachomatis in pregnancy. Am J Obstet Gynecol. 2001 Jun;184(7):1352-4; discussion 1354-6. PubMed
- 12. Kacmar J, Cheh E, Montagno A, Peipert JF. A randomized trial of azithromycin versus amoxicillin for the treatment of Chlamydia trachomatis in pregnancy. Infect Dis Obstet Gynecol. 2001;9(4):197-202. PubMed
- 13. Arguedas A, Emparanza P, Schwartz RH, Soley C, Guevara S, de Caprariis PJ, Espinoza G. A randomized, multicenter, double blind, double dummy trial of single dose azithromycin versus high dose amoxicillin for treatment of uncomplicated acute otitis media. Pediatr Infect Dis J. 2005 Feb;24(2):153-61. PubMed
- 14. Luft BJ, Dattwyler RJ, Johnson RC, Luger SW, Bosler EM, Rahn DW, Masters EJ, Grunwaldt E, Gadgil SD. Azithromycin compared with amoxicillin in the treatment of erythema migrans. A double-blind, randomized, controlled trial. Ann Intern Med. 1996 May 1;124(9):785-91. PubMed
- 15. Dunne MW, Latiolais T, Lewis B, Pistorius B, Bottenfield G, Moore WH, Garrett A, Stewart TD, Aoki J, Spiegel C, Boettger D, Shemer A. Randomized, double-blind study of the clinical efficacy of 3 days of azithromycin compared with co-amoxiclav for the treatment of acute otitis media. J Antimicrob Chemother. 2003 Sep;52(3):469-72. Epub 2003 Jul 29. PubMed
- 16. Henry DC, Riffer E, Sokol WN, Chaudry NI, Swanson RN. Randomized double-blind study comparing 3- and 6-day regimens of azithromycin with a 10-day amoxicillin-clavulanate regimen for treatment of acute bacterial sinusitis. Antimicrob Agents Chemother. 2003 Sep;47(9):2770-4. PubMed
- 17. Ferwerda A, Moll HA, Hop WC, Kouwenberg JM, Tjon Pian Gi CV, Robben SG, de Groot R. Efficacy, safety and tolerability of 3 day azithromycin versus 10 day co-amoxiclav in the treatment of children with acute lower respiratory tract infections. J Antimicrob Chemother. 2001 Apr;47(4):441-6. PubMed
- 18. Jennings MB, McCarty JM, Scheffler NM, Puopolo AD, Rothermel CD. Comparison of azithromycin and cefadroxil for the treatment of uncomplicated skin and skin structure infections. Cutis. 2003 Sep;72(3):240-4. PubMed
- 19. Block SL, Cifaldi M, Gu Y, Paris MM. A comparison of 5 days of therapy with cefdinir or azithromycin in children with acute otitis media: a multicenter, prospective, single-blind study. Clin Ther. 2005 Jun;27(6):786-94. PubMed
- 20. Alvarez Gutie’rrez FJ, Soto Campos G, del Castillo Otero D, Sa’nchez Go’mez J, Caldero’n Osuna E, Rodri’guez Becerra E, Castillo Go’mez J. A randomized comparative study of 3 days of azithromycin treatment and 10 days of cefuroxime treatment in exacerbations in patients with chronic obstructive pulmonary disease Med Clin (Barc). 1999 Jul 3;113(4):124-8. PubMed
- 21. Skerk V, Schonwald S, Krhen I, Banaszak A, Begovac J, Strugar J, Strapac Z, Vrsalovic R, Vukovic J, Tomas M. Comparative analysis of azithromycin and ciprofloxacin in the treatment of chronic prostatitis caused by Chlamydia trachomatis. Int J Antimicrob Agents. 2003 May;21(5):457-62. PubMed
- 22. Khan WA, Seas C, Dhar U, Salam MA, Bennish ML. Treatment of shigellosis: V. Comparison of azithromycin and ciprofloxacin. A double-blind, randomized, controlled trial. Ann Intern Med. 1997 May 1;126(9):697-703. PubMed
- 23. Gruber F, Brajac I, Jonjic A, Grubisic-Greblo H, Lenkovic M, Stasic A. Comparative trial of azithromycin and ciprofloxacin in the treatment of gonorrhea. J Chemother. 1997 Aug;9(4):263-6. PubMed
- 24. Amsden GW, Baird IM, Simon S, Treadway G. Efficacy and safety of azithromycin vs levofloxacin in the outpatient treatment of acute bacterial exacerbations of chronic bronchitis. Chest. 2003 Mar;123(3):772-7. PubMed
- 25. D’Ignazio J, Camere MA, Lewis DE, Jorgensen D, Breen JD. Novel, single-dose microsphere formulation of azithromycin versus 7-day levofloxacin therapy for treatment of mild to moderate community-acquired Pneumonia in adults. Antimicrob Agents Chemother. 2005 Oct;49(10):4035-41. PubMed
- 26. Henry DC, Kapral D, Busman TA, Paris MM. Cefdinir versus levofloxacin in patients with acute rhinosinusitis of presumed bacterial etiology: a multicenter, randomized, double-blind study. Clin Ther. 2004 Dec;26(12):2026-33. PubMed
Published: March 31, 2008
Last updated: January 09, 2010




USP grade Azithromycin can be purchased from
http://aquaticpharmacy.com/product-info
Read the F.A.Q. on this website. It will answer most of your questions regarding quality.
are these antibiotics safe for human consumption and in what doses do you take them?
It appears you mix them in water?
WHERE CAN i BUY aZITHROMYCIN W/O PRESCRIPTION.
can i get this over the counter?????
thank you.