The following is excerpted from my upcoming book, Armageddon Medicine.
Thyroid disease – Hypothyroidism (Low thyroid)
The question of treating low thyroid in a post-apocalyptic world is a common one. If Synthroid becomes unavailable, is a hypothyroid person doomed?
The short answer is: likely not – so read on.
Hypothyroidism (low thyroid, or thyroid insufficiency) encompasses a wide spectrum of problems, from asymptomatic (subclinical) hypothyroidism, to severe disease and coma. Only once in my 30-year medical career have I seen a patient obtunded from hypothyroidism, and I’ve never seen a patient with an iodine-deficiency goiter, though that disease may resurface after global catastrophe.
For simplicity sake, I’ll divide low-thyroid disease into two main classes: those with an absolute deficiency of thyroid hormones and those with a partial deficiency. People with no thyroid hormone whatsoever must receive replacement therapy or they will gradually succumb to severe thyroid deficiency (fatigue, low heart rate, slowed thinking, swollen legs, dry skin, hair loss, and possible coma and death). People with a partial deficiency may live for years or even decades with minimal or no symptoms.
The real question is: which sort of patient are you?
Most people won’t know the answer to this question. You can, however, determine the answer with a little investigation.
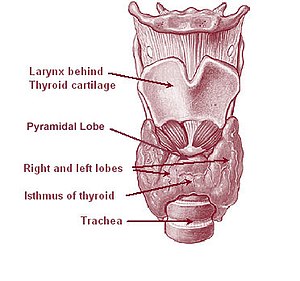
Absolute thyroid deficiency is mainly caused by two conditions: severe, intrinsic thyroid disease or as a result of treatment for hyperactive thyroid (high thyroid, Grave’s disease). Patients who have undergone total thyroidectomy or total thyroid ablation via radiation for a hyperactive thyroid should, theoretically, have no remaining functional thyroid tissue. This is not always the case, since some doctors treat hyperthyroid disease with a sub-total thyroidectomy or incomplete irradiation, aiming to leave sufficient thyroid tissue to avoid the need for replacement therapy.
Much more common is partial thyroid deficiency. To determine this, what doctors actually measure is the serum TSH level (thyroid stimulating hormone). TSH is produced by the pituitary, and as the name implies, TSH stimulates the thyroid to make thyroid hormone via a fine-tuned feedback system. If your serum thyroid level drops a bit low, the pituitary responds by producing more thyroid stimulating hormone, which in turn causes the thyroid gland to increase output of thyroid hormone (assuming there is thyroid tissue to stimulate). If your serum thyroid hormone level increases, TSH levels drop.
Nowadays most patients with hypothyroidism are diagnosed by an elevated TSH level rather than by symptoms. Sure, a patient may complain of fatigue, but who isn’t tired? I’ve had many patients with a mildly elevated TSH level who were placed on thyroid replacement therapy, either by myself or another physician, who felt absolutely no different taking Synthroid. A serum TSH level is a common screening blood test for middle-aged and older people undergoing a routine exam. Therefore mild hypothyroidism is thus often identified in patients who had no clue anything was wrong. Another name for this problem is ‘subclinical hypothyroidism,’ that is, too mild to cause symptoms.
The normal range for TSH varies from lab to lab, but is approximately 0.3 to 5.0 mIU/L. Patients are commonly placed on thyroid replacement therapy when their TSH is elevated a few points, even if they have no symptoms. However, this practice is controversial. Per a review article in The American Family Physician, “In current randomized controlled trials, levothyroxine replacement therapy for subclinical hypothyroidism did not result in improved survival or decreased cardiovascular morbidity. Data on health-related quality of life and symptoms did not demonstrate significant differences among intervention groups. Some evidence indicates that levothyroxine replacement improves some parameters of lipid profiles and left ventricular function.” (Am Fam Physician. 2008 Apr 1;77(7):953-955, online at: http://www.aafp.org/afp/2008/0401/p953.html)
My own experience confirms this data. So if you won’t feel better or live longer, and if you are not experiencing symptoms of hypothyroidism, patients in this category probably don’t require treatment.
However, there are patients whose TSH levels are elevated by 20, 30, or even 100 points. These patients are likely to exhibit symptoms and on blood testing are likely to show decreased levels of serum thyroid hormone. Common symptoms of hypothyroidism include: weakness, dry or coarse skin or hair, fatigue or lethargy, swollen eyelids or face, feeling cold, slowed speech or thinking, and constipation. Of course, many patients have one or more of these symptoms and do not have any thyroid disease. However, patients with decreased thyroid function will improve if given thyroid supplementation.
Future installments of this topic will include:
- Old, current, and future treatment of hypothyroidism
- Figuring out what type of thyroid disease you have
- Stockpiling medication
- Alternative and complementary medicine
For more answers to your thyroid questions, see HYPOTHYROIDISM – Answers for the End of the World.




I read taking thyroid meds can cause bone to thin and the Dr. s do not know why…
A few years ago, my mother decided to stop taking her thyroid medication and began taking gugulipid. Her TSH soared. She had dry skin and hair, an extremely puffy face, was always cold, had mental confusion and slurred speech. I dragged her back to the doctor, tossed her gugulipid, and she was put back on Synthroid. After a few months, her symptoms subsided.
With that in mind, the time to test the effectiveness of any supplement or medication (or ability to withstand the lack thereof) is BEFORE the poop hits the fan, when you can still see your doctor and get appropriate blood tests done.
I had to look that one up – gugulipid. According to Pharmacotherapy. 2001;21(4) © 2001 Pharmacotherapy Publications available online at http://www.medscape.com/viewarticle/409698 –
“Gugulipid, also known as guggul or gum guggula, is the gum extract of the mukul myrrh tree (Commiphora mukul), which is native to India. It traditionally is used to reduce weight and treat arthritis and nodulocystic acne. The presumed hypolipidemic constituents are Z- and E-guggulsterones. These constituents may act by decreasing hepatic steroids, which increases compensatory cholesterol biosynthesis and subsequently causes increased plasma LDL particle catabolism. Other potential mechanisms are thyroid stimulation and antiinflammatory effects.”
This is an excellent example of how a tiny snippet of medical supposition gets translated into generalized use of an herb, often inappropriately.
I agree with Charles that now is the time to undergo whatever testing is needed to understand any health problems a person may have. Thanks for the comment.
I find this interesting – mainly because Levoxyn (sp?) is the only medication I take and I’m 75 years of age. I asked to get off the meds. and my dr. said NO. She based her opinion on lab results but I do ot know what they were – I DO have the symptoms mentioned in your article…
If you really want to understand your situation, ask your doctor for a longer appointment to explain it to you thoroughly, say a 15-20 minute appointment. (I talk about this alot in my book, 101 Ways to Save Money on Health Care.)
The trouble with monitoring symptoms is they can be quite nonspecific or possibly due to other causes as well. For a person whose blood tests are normalized, symptoms are likely not due to thyroid disease.
Patients have a right to understand their blood tests, and also the consequences of discontinuing medication. Your doctor no doubt understands the situation and may simply need to explain it in more detail. You may want to ask whether you have an absolute deficiency of thyroid production, or a partial deficiency, and whether your T3 and T4 levels are low, or if your TSH is elevated. I’ll be posting more on this topic in the near future.
Cure for hypothyroidism? What to take naturally?
Pingback: Thyroid disease – Hypothyroidism (low thyroid) – Part 2 | Armageddon Medicine