The following is second in a series contributed by Pete Farmer, who holds advanced degrees in research biology and history, and is also an RN and EMT.
* * *
Having examined the physical and chemical properties of water in the first installment of this series, let us turn our attention to less-theoretical concerns, namely the physiological role of water in humans, hydration in extreme environments, and related matters.
Water governs or supports nearly every aspect of our anatomy and physiology – including acid-base chemistry, electrolyte balance, intra- and extracellular transport mechanisms, cell structure, and much more. Almost without exception, the biochemistry of the human body takes place in water. If deprived of it, the reactions which sustain life falter, and then cease altogether.
The human body is typically composed of approximately 55-70% water by weight, and may range as low as 45% or as high as 75% depending on numerous variables. These include hydration level/fluid intake, age, sex, weight, state of health, level of activity, weather and climate (ambient air temperature, barometric pressure, relative humidity and wind), altitude, stress level, toxic burden and metabolic waste load, solute concentrations within various body spaces, and many other factors.
Diffusion governs the movement of many substances within the body and in nature. It is defined as the passive movement of molecules or particles along a concentration gradient, or from regions of higher to regions of lower concentration – until the concentration is constant. Put a drop of colored iodine solution in a glass of clear water, and the iodine will spread until the water is a dilute, uniform color. This is a simple example of diffusion.
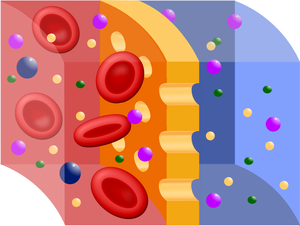
A special form of diffusion common within biological systems is osmosis, which is the movement of water/fluid from an area of high concentration to an area of low concentration, across a semipermeable membrane (i.e., one which allows the passage of certain, especially small, molecules or ions/charged atoms but acts as a barrier to others). A solute is defined as a dissolved solid substance in solution. For example, pure water contains no solutes, common sea or salt water contains dissolved solids such as sodium chloride (NaCl) and potassium chloride (KCl). Divided by a cell or other semipermeable membrane – such as a capillary wall – found in the body, water will flow by osmotic diffusion from the pure water compartment into the compartment containing salt water (i.e., containing solutes), until the concentration is equalized in both compartments. Salts, proteins, and other substances which cause the osmotic diffusion of water in solution are termed osmotically-active. Why is this important in everyday life? Read on: osmosis has very consequential, real-world effects vis-à-vis survival hydration – which are covered below. For now, the most important lesson is to remember that in the body, water follows salts.
Internal fluid balance is homeostatically-controlled in a dynamic equilibrium. Fluid balance is maintained within functional range by a complex system of biochemical checks-and-balances and feedback mechanisms. The hormones Anti-diuretic hormone (ADH, also known as vasopressin) and Aldosterone play major roles.
Changes of the concentration of solutes in the blood, indicative of water excess or depletion (dehydration), are sensed by specialized cells in the hypothalamic gland called osmoreceptors. Dehydration – caused by excessive sweating, hemorrhage, vomiting or diarrhea, or insufficient fluid intake – triggers the renin-angiotensin-aldosterone system (RAAS), which causes blood vessels to constrict, elevating blood pressure. The release of the hormone aldosterone from the adrenal glands causes reabsorption of sodium and water into the blood, also elevating blood volume and pressure. Antidiuretic hormone (also called vasopressin or ADH) is secreted by the pituitary gland when specialized pressure receptors in the blood vessels detect a decrease in blood plasma volume and pressure. ADH acts upon the kidneys to cause increase reabsorption of water back into the bloodstream following filtration, thereby concentrating urine. The activation of the above systems triggers the sensation of thirst. Once sufficient blood volume and pressure is restored, usually by fluid intake, feedback control down-regulates these systems.
Infants have the highest percentage of H2O by weight – about 75%; this figure declines with age. In the adult male, water accounts for about 60% of weight; in the adult female, about 55% – the difference due mostly to the generally higher level of subcutaneous adipose tissue in females compared to males. Adipose tissue contains almost no water; therefore, as adipose tissue as a percentage of body mass increases, the relative percentage of water weight decreases. Fat people have a smaller proportion of water than do lean people.
In the healthy human adult at rest, daily water intake/gain equals water excretion/loss – around 2500 ml (2.5L)/day, or about 0.66 U.S. gallons.
Sources of water gain/intake = metabolic reactions (200mL), ingested foods (700ml), ingested liquids (1600ml). Sources of excretion/loss = GI tract digestion (200ml), insensible water loss – evaporative loss on skin surface, perspiration, and expired air (800ml), renal filtration/urination (1500ml). Sexually-mature woman lose an additional ~ 50ml/day due to vaginal secretions, and will also lose water during menstrual blood loss.
Electrolytes are defined chemically as any substance containing free ions (positively or negatively charged atoms) which allow a solution to conduct electricity. In practical terms, they are usually acids, bases or salts. All living things are dependent on an intricate and subtle balance of electrolytes within cells and also the extracellular fluids that bathe them. The most common and important electrolytes in the human body are sodium (Na+), potassium (K+), calcium (Ca2+), magnesium (Mg2+), chloride (Cl−), hydrogen phosphate (HPO42−), and hydrogen carbonate (HCO3−). Electrolytes allow the storage of electric potential energy within excitatory cells and tissues – such as skeletal and cardiac muscle and neurons. Unbalanced or insufficient electrolytes figure prominently in many illnesses and disorders, and if uncorrected, result in death.
Medically, there are at least three types of dehydration (fluid deficiency in the body) – due to the loss of electrolytes (primarily inorganic salts) alone, due to loss of fluid volume alone, or a combination of both. Differentiation between these should be left to a qualified medical professional, and will probably require a detailed physical exam, and diagnostic testing.
Dehydration is often accompanied by electrolyte depletion, especially in cases involving severe diarrhea or vomiting, prolonged heat exposure, burns and thermal trauma, prolonged fasting, anorexia nervosa/bulimia, and/or malnutrition and rapid weight loss; it is also a diagnostic indicator of many illnesses, such as diabetes types I and II, uremia, proteinuria (protein in the urine), and others. Uncontrolled or inadequately diabetes, for example, will manifest frequent urination (polyuria) and severe thirst (polydipsia).
A couple of other useful terms that pertain to the discussion of water balance: A diuretic is a substance which promotes urine formation or urination. Many commonly available foods, beverages, and over-the-counter dietary supplements contain diuretics, often stimulants such as caffeine. Alcohol, coffee, tea, caffeine-containing soda, chocolate, and dietary supplements containing now-banned stimulants such as ephedra are all diuretics. Common OTC cold medicines, containing stimulants such as ephedrine/ pseudoephedrine, also act as diuretics. In practical terms, those attempting to rehydrate themselves should avoid these to the degree possible. Lay readers may be familiar with so-called “water pills,” which are diuretic drugs formulated to cause excretion of excess body fluid in cases of hypertension and other illnesses involving fluid overload. Furosemide (Lasix) and hydrochlorothiazide (HCTZ) are commonly prescribed diuretic medications. Do not attempt to self-diagnose or treat hypertension or chronic illnesses related to fluid balance – these substances are to be used under the care of a qualified physician and pharmacist only. Nor should these compounds be use or abused to promote weight loss. Abuse of diuretic compounds can have serious or fatal consequences.
The Signs and Symptoms of Dehydration
Signs & symptoms of dehydration generally become noticeable after the body has lost 2-5% of its normal fluid volume. Mild dehydration is often manifested as:
- Muscle cramping
- Dry skin, eyes and mouth
- Dizziness upon standing (orthostatic hypotension)
- Thirst (appears relatively late as an indicator, as noted above)
- Urine is concentrated, dark-yellow in color, of pronounced odor, and urination is reduced in volume and frequency. Conversely, well-hydrated individuals have light amber or nearly clear urine.
- Constipation
- Decreased athletic performance
- Irritability, fatigue
Intermediate- or acute (5-15% water loss) dehydration is characterized by:
- Extreme lethargy and/or sleepiness
- Weight loss
- Headache
- Nausea
- Numbness or tingling in one’s extremities (paresthesia)
- Sunken fontanel (soft spot) in infants
- Dizziness upon standing (orthostatic hypotension)
- Altered mental status as above, except more severe – confusion/disorientation, hallucinations*
- Further diminished urine output or absence of urine
- Loss of consciousness/fainting
- Sunken eyes, little or lacrimation (tear formation)
- Possible lack of perspiration, elevated body temperature
- Increased heart rate, rapid and thready pulse, increased respiration rate
- At 10-15%, decreased skin turgor is evident (skin wrinkles and shrivels), muscle spasm or seizures may occur, and vision is altered.
- Loss of more than 15% of body water is frequently fatal
* – A mini-mental status check can be performed by assessing the subject’s cognition and awareness of his/her surroundings. “Alert and oriented x 3” indicates that the patient is alert and aware of person, place and time (who they are, where they are, and what day/time it is).
Fluid Replacement
Fluid replacement is the treatment for dehydration. If oral rehydration is inadequate, intravenous (IV) fluid replacement may be indicated; IV fluid resuscitation should be performed only by a qualified medical professional. Oral hydration therapy can be administered by frequent small amounts of clear fluid should be used. Clear fluids include water, clear broths, popsicles, Jell-O, and electrolyte-containing fluids such as sports drinks (Gatorade, Powerade, etc.) and specialized fluids such as Pedialyte. Avoid fluid replacement with diuretics – especially alcohol – which complicates both diagnosis and treatment. Do not use sea/salt water as a substitute for fresh water – even if it is the only water available; it can be fatal. Concentrated in solutes, sea water actually draws water from the body, dehydrating it further and worsening electrolyte imbalances.
If brackish or contaminated fresh water is all that is available, a cost-benefit judgment will have be made concerning its use (more on this problem in future articles).
If the patient is unable to keep down small slips of replacement fluid, and regurgitates them via vomiting or experiences diarrhea as a result, immediately call 911. Do not attempt to force-feed oral hydration to an unconscious person, or anyone whose airway may be compromised. Medical attention should also be sought immediately if oral rehydration fails to relieve signs and symptoms of acute dehydration. Intravenous fluid resuscitation therapy is advanced life support, and should be carried out only by trained personnel, except in the most-dire circumstances where qualified medical help is unavailable. This is especially true of electrolyte imbalances, whose diagnosis and treatment are often subtle and complex. In these cases, emphasis should be on getting the affected person to a fully-equipped medical facility as soon as possible.
Conclusion
In upcoming installments, we will continue to explore water and medical survival, including methods of water treatment, improvised collection of water in extreme environments, water-borne illnesses and how to avoid them, and much more.
Copyright © 2011 Peter Farmer
Related articles
- Osmolality – blood – All Information (umm.edu)
- Diabetes insipidus – All Information (umm.edu)
- Diabetes insipidus – nephrogenic – All Information (umm.edu)






Great article, thanks! Can you tell me if 8 glasses of water a day is still recommended? I vaguely remember reading that there was a debate that it might be more than needed and unnecessarily taxing to the kidneys. Also, any non-diuretic liquid I drink counts toward that total, including milk, right?
[Doc Cindy answers . . . Yes – eight glasses of fluids daily (about 2 liters) is the standard recommendation for a healthy, average-size person. Overall, men need a little more than women, based on size. When doctors order IV fluid replacement for an adult, a typical rate is 75-100 mL per hour, yielding 1.8 – 2.4 liters/day. Under certain circumstances – for example, fever, diarrhea, sweating, or diuretic therapy – people may need more. Certain patients – most notably those suffering from heart or kidney failure – may require somewhat less. For a healthy patient, extra fluid does not tax the kidneys. I have known many individuals who drink significantly less than 2 liters of fluid daily with no ill effects, though inadequate intake does predispose to kidney stones, dehydration, and constipation. The topic of fluid replacement therapy will be addressed in greater detail in a future post.]